Skin and nail fungus treatment using compounds

Fungal infections in the United States
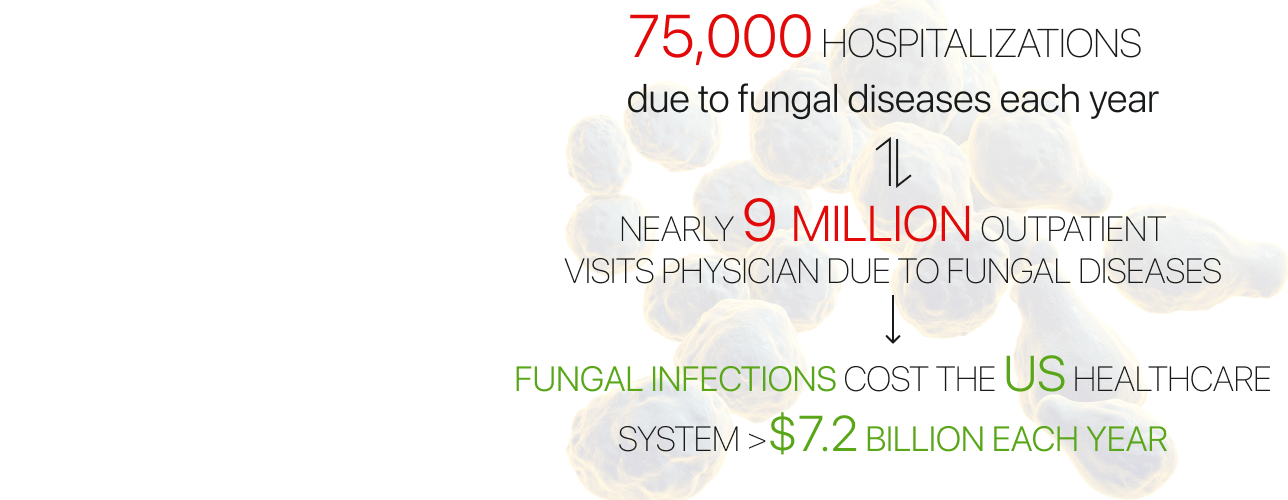
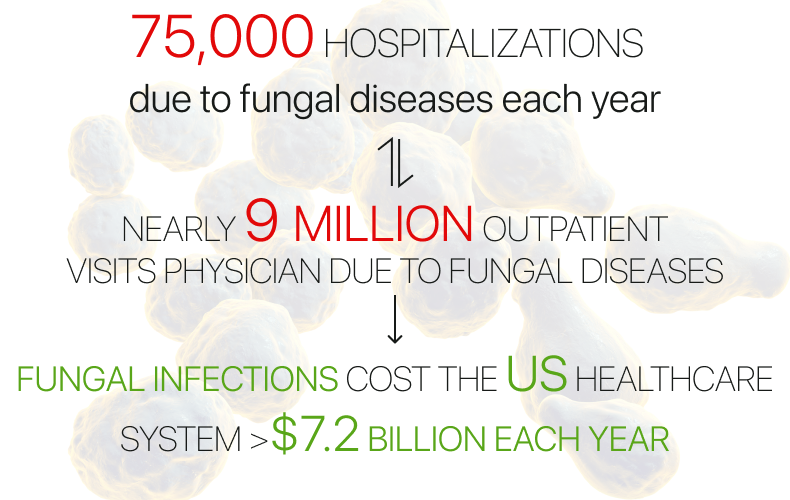
Fungus is very common and not always visible to the naked eye, and it can be everywhere. On surfaces, in the soil or air, on our skin, or inside our body. Fungal infections cost the US healthcare system over $7.2 billion each year and cause substantial rates of disease and death. According to the Center for Disease Control and Prevention, more than 75,000 hospitalizations and nearly 9 million outpatient visits occur each year due to fungal diseases. As for the number of deaths, an estimated 7,199 deaths from fungal diseases occurred in 2021. We may underestimate this disease, but there are millions of fungal species that can affect each of us, and many of them can have serious consequences for human health.
When the skin comes into contact with an adverse fungus, the infection can cause a rash. A fungal rash can appear on any part of the human body, including nails, and mucous membranes, it is also common in areas with skin folds, such as the groin, buttocks, or thighs. It mainly manifests itself in a rash that causes itching and burning, asthma or allergies, lung infections (pneumonia), symptoms similar to the flu or tuberculosis, bloodstream infections, and meningitis… Of course, the manifestation of symptoms differs depending on the type of fungus that a person is affected by.
Interesting fact: More than 200 species of fungi live on our feet. Even if you love to take long baths, this does not negate the fact that their favorite spots to colonize and grow are the heel (80 types found), between the toes (40), and beneath the toenails (60). Most of these fungi are totally harmless, however, if they multiply, then infections can occur and should be treated.


People with certain diseases take medications that can cause side effects and weaken their immune system, which makes them more susceptible to fungal infections. Diseases such as diabetes, HIV, cancer, and poor circulation weaken the human immune system, making it much harder for the body to fight infections.
Equally interesting, COVID-19 is likely to increase the risk of fungal infections. This is happening due to covid treatment, which again weakens the human immune system. This was noticed by researchers who tracked the trend of increasing mortality from fungal diseases in 2021–2022 compared to previous years, primarily driven by COVID–19–associated deaths. Specialists who have studied the topic of Covid and fungus have concluded that Coronavirus disease can increase the risk of developing severe fungal infections due to immune system dysfunction.
Fungus medical conditions and diagnoses
Mega Aid has developed a number of topical compounds for treating the following fungus conditions: Tinea pedis, Tinea corporis (Ringworm), Tinea faciei, Tinea barbae, Tinea capitis, Tinea cruris (Jock Itch), Tinea manuum, Tinea unguium (onychomycosis), Interdigital maceration.


Tinea pedis is a fungal skin infection of the foot that usually begins between the toes. Tinea pedis is usually acquired by means of:
– Direct contact with the causative organism – Walking barefoot in locker rooms or swimming pool facilities
– Wearing occlusive footwear (shoes or boots that enclose the feet)
Tinea pedis can affect one or both feet and may present with itching, burning, or dryness of the skin.
Tinea corporis refers to infections in sites of the body such as the groin, face, or hand. Infection may occur by direct skin contact with an infected individual or animal or from secondary spread due to other infected sites such as the scalp or feet. Tinea corporis may present as an itchy, round, red, or hyperpigmented flat patch of skin with a raised scaly border.
Tinea faciei is a dermatophyte infection of facial skin devoid of terminal hairs. Tinea faciei may present as small, scaly papules (small, well-defined bump in the skin) that can form into annular plaques (ring-shaped lesions). This disease is related to tinea corporis and can be acute or chronic. The condition of infection may worsen under the influence of sun exposure.
Tinea barbae is a dermatophyte infection involving beard hair in adolescent and adult males. This is a rare fungal infection that most often affects the face and hair follicles near the beard and mustache. Tinea barbae infections spread through direct contact with animals. The most common symptoms that appear are itchy, red, ring-shaped rashes on the outer layer of the skin. Most often these rashes appear on the cheeks, chin, or neck. In the worst cases, people may develop a fever and swollen lymph nodes.
Tinea capitis is an infection of the scalp, that often presents with itchy, scaling areas of hair loss. Tinea capitis primarily occurs in children. Signs of this disease can include unpleasant itchy, scaly, bald patches on the head. Patches can slowly get bigger and have black dots where the hair has fallen off.
Tinea cruris. Infection often results from the spread of the dermatophyte infection from concomitant tinea pedis. Predisposing factors include copious sweating, obesity, diabetes, and immunodeficiency. Tinea cruris often begins with a red or hyperpigmented patch on the inner thigh. The infection spreads centrifugally, with partial central clearing and a slightly elevated, border. Tinea cruris is treated with topical anti-fungal drugs.
Tinea manuum is a fungal infection that usually affects one hand. Patients present with a hyperkeratotic eruption (when the thickness of the stratum corneum is increased) on the palm or plaques similar to tinea corporis on the palm of the hand. This disease starts to affect a person`s palm and can spread to the fingers and the back of the hand. Infected areas are red, itchy, and have a scaly appearance. Tinea manuum can also cause blistering on the edges of the fingers or palm.
Tinea unguium or Onychomycosis is a fungal infection that affects fingernails or toenails. It occurs most often in adults but may also occur in children. Tinea unguium presents with nail discoloration, splitting of the nail plate, and nail destruction. Infection may potentially spread to other body sites.
Interdigital maceration appears on the skin when the water content is disordered because of sweating or it appears once the evaporation of moisture between the toes is impaired.
he skin becomes white and ‘soggy’ between the toes. Excessive moisture alters the normal microbiological flora which increases the risk of a secondary bacterial or fungal infection. Risk factors include excessive sweating, poor foot hygiene practices, or too much footwear use.
Drug classes used for fungus treatment
A general approach to prevention is to keep the affected area dry and clean, limit exposure to the infected reservoir, reduce the risk of secondary bacterial infection, and limit the spread of the infection to other sites or individuals.
Treatment approach. Topical treatment is preferred, this method is used by Mega Aid in the combat against fungus. Treatment is usually for a couple of weeks, but sometimes can be continued after the resolution of symptoms for up to a year. Below you can explore the main drug classes which we use in the production of customized medicines.
All compounds are unique and are made taking into account the individual’s characteristics. The doctor writes a prescription based on the patient’s diagnosis and specific case; after receiving the prescription, our pharmacists make the compound treatment in our laboratories.
If you are a healthcare provider and you want to improve patient outcomes with Mega Aid, contact us to connect with a dedicated Pharmacy Liaison who can discuss our formulation
capabilities that are appropriate to each patient’s individualized condition and needs.
How medication therapy management can improve fungus treatment
Recuperation includes not only the right treatment but also the proper implementation of the doctor’s instructions for effective recovery. That is the correct usage of medicines, dosage, timing, etc.
Unfortunately, not every patient adheres to the requirements that the doctor tells them about. According to FDA statistics, about 50% of people do not adhere to the correct treatment regimen, and 20% to 30% of new prescriptions are never filled at the pharmacy. Of course, this does not lead to anything good, but only to health complications and hospitalizations that could have been prevented.
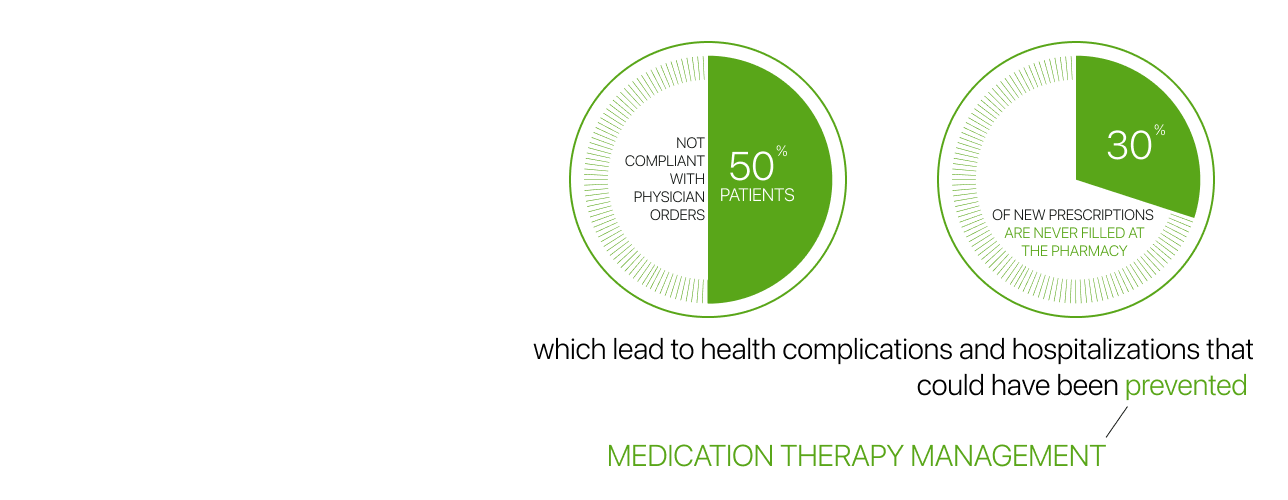
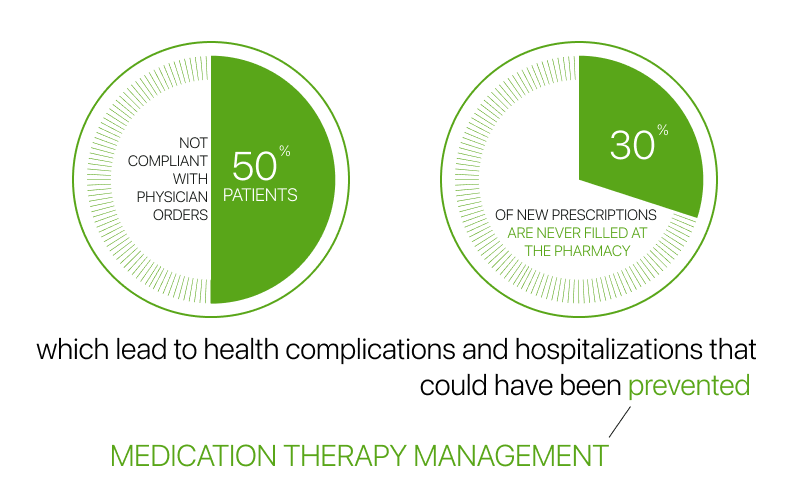
Mega Aid long ago realized the scale of the problem, so we developed our own in-house medication therapy management program. It is helpful for healthcare providers, because they can be sure that their patients treatment compliance, and health condition is responsibly monitored. It is also beneficial for the patients because they can always count on our support, education, reminders, and tracking of their health.
This is how medication therapy management works in Mega Aid:
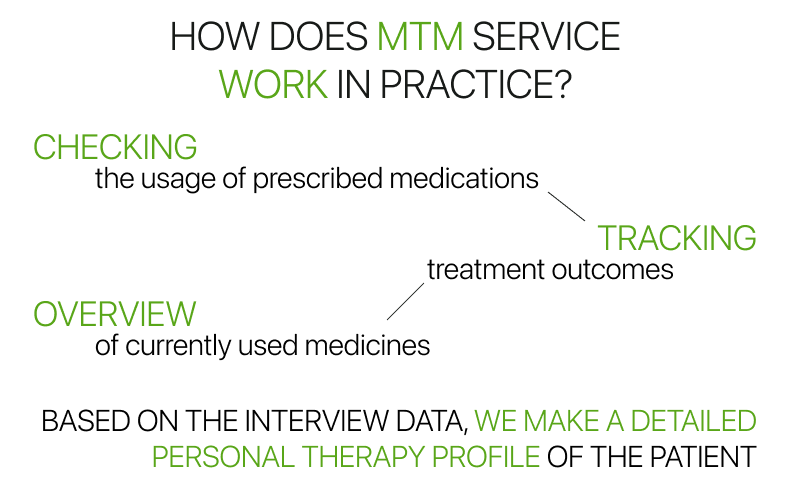
1. Checking the usage of prescribed medications
After receiving the prescribed compounds, our Patient Care Coordinators ask whether the patient has used the medication. We record how many times and in what dosage. If the patient did not take medications or used the medication not according to the prescription – we speak with the patient about usage to improve their literacy about proper medication usage by educating them.
2. Tracking treatment outcomes
During the treatment, we record in our database patients’ outcomes: how the patient’s condition has changed after using the compound medications. In case of side effects or other reactions, we record everything in the database for further formulation improvements with the physician.
3. Overview of currently used medicines
We ask whether the patient currently uses any other medicines. If the answer is ”yes”, then we request to specify which ones, in what doses, and how many times per day. Thereby, we control drug tolerances and compare used medications with disease states in our database.
We enter all the necessary information into our database that will be important for further treatment improvement.
All this allows us to see the patient’s whole therapeutic picture, taking into account all indicators including allergies, and drug tolerance in interaction with other drugs to avoid side effects and negative consequences. We are always in touch with the patient to improve the treatment plan in collaboration with the healthcare provider.
Over 600 Healthcare Providers already rely on Mega Aid, join our mission to improve patient outcomes, book a meeting with one of our dedicated Pharmacy Liaisons.



