What Data or Reporting Can Medication Therapy Management Provide for Value-Based Medicine Programs?

Medication Therapy Management (MTM) is rapidly becoming a cornerstone in value-based medicine programs. By integrating MTM into care pathways, healthcare providers, payers, and pharmacies can collect and report actionable data that improves patient outcomes and supports value-driven care.
At Mega Aid Compounding Pharmacy, our advanced MTM services are designed to enhance medication adherence, monitor treatment progress, and provide robust reporting for value-based medicine programs. This page explores the types of data MTM generates, how it supports value-based care initiatives, and how Mega Aid leads in actionable, results-driven reporting.
- Overview: MTM & Value-Based Medicine
- Key Data Elements MTM Programs Provide
- Reporting Metrics for Value-Based Programs
- Mega Aid’s MTM Data & Reporting Solutions
- Case Study: Diabetes Adherence Program
- Data Visualizations & Sample Reports
- FAQs
- How to Get Started
Overview: MTM & Value‑Based Medicine
Medication Therapy Management (MTM) involves personalized clinical interventions to optimize medication use, improve adherence, and address barriers that affect patient outcomes. Value-based medicine rewards providers for improved patient outcomes and reduced healthcare costs, making data-driven MTM a crucial component.
How MTM Supports Value-Based Care:


Key Data Elements MTM Programs Provide
MTM programs capture and report a range of data points vital for value-based medicine initiatives. Below is a summary table of core MTM data elements:
| Data Element | Description | Value for VBP* |
|---|---|---|
| Medication Adherence | % of days patient takes medication as prescribed (PDC) | High (CMS, payers) |
| Gaps in Therapy (GIT) | Days without medication coverage | High |
| Medication Review Outcomes | Recommendations, therapy adjustments, interventions | Medium |
| Patient Education/Coaching | Documentation of counseling, disease education | Medium |
| Clinical Parameters | A1c (diabetes), BP, LDL, etc. | High |
| Cost Data | Plan-paid, patient-paid, copayments | Medium |
| Adverse Events/Side Effects | Tracking and reporting | High |
| Patient Satisfaction | Survey scores, qualitative feedback | Medium |
| Provider Communication | Interventions, outcome reporting | High |
*VBP = Value-Based Programs
Reporting Metrics for Value‑Based Programs
Common MTM Metrics Tracked & Reported:
- Proportion of Days Covered (PDC): Percentage showing how consistently a patient takes their medication.
- Gaps in Therapy (GIT): Number of days a patient is not covered by therapy.
- Clinical Outcomes: Changes in lab values (A1c, BP), hospitalizations, ER visits.
- Cost Metrics: Pharmacy spend, medical spend, cost avoidance.
- Patient Engagement: Participation in coaching, follow-up appointments.
- Intervention Acceptance Rate: % of MTM recommendations accepted by providers.
- Health Disparity Reduction: Outcomes stratified by gender, age, or condition.
Mega Aid's MTM Data & Reporting Solutions
At Mega Aid Compounding Pharmacy, we:
- Before compounding, we perform Drug Utilization Review – checking all the medications the patient currently takes, even those prescribed by other providers, to avoid negative drug-to-compound interactions
- Educate patients on how to use medications correctly via phone and provide video instructions on YouTube
- Track patients’ medication adherence and clinical outcomes in real-time.
- Identify patients at risk for non-adherence or complications.
- Report treatment progress and outcomes directly to providers to adjust the therapy if needed.
- Support closed-loop communication with providers for continuous care improvement.
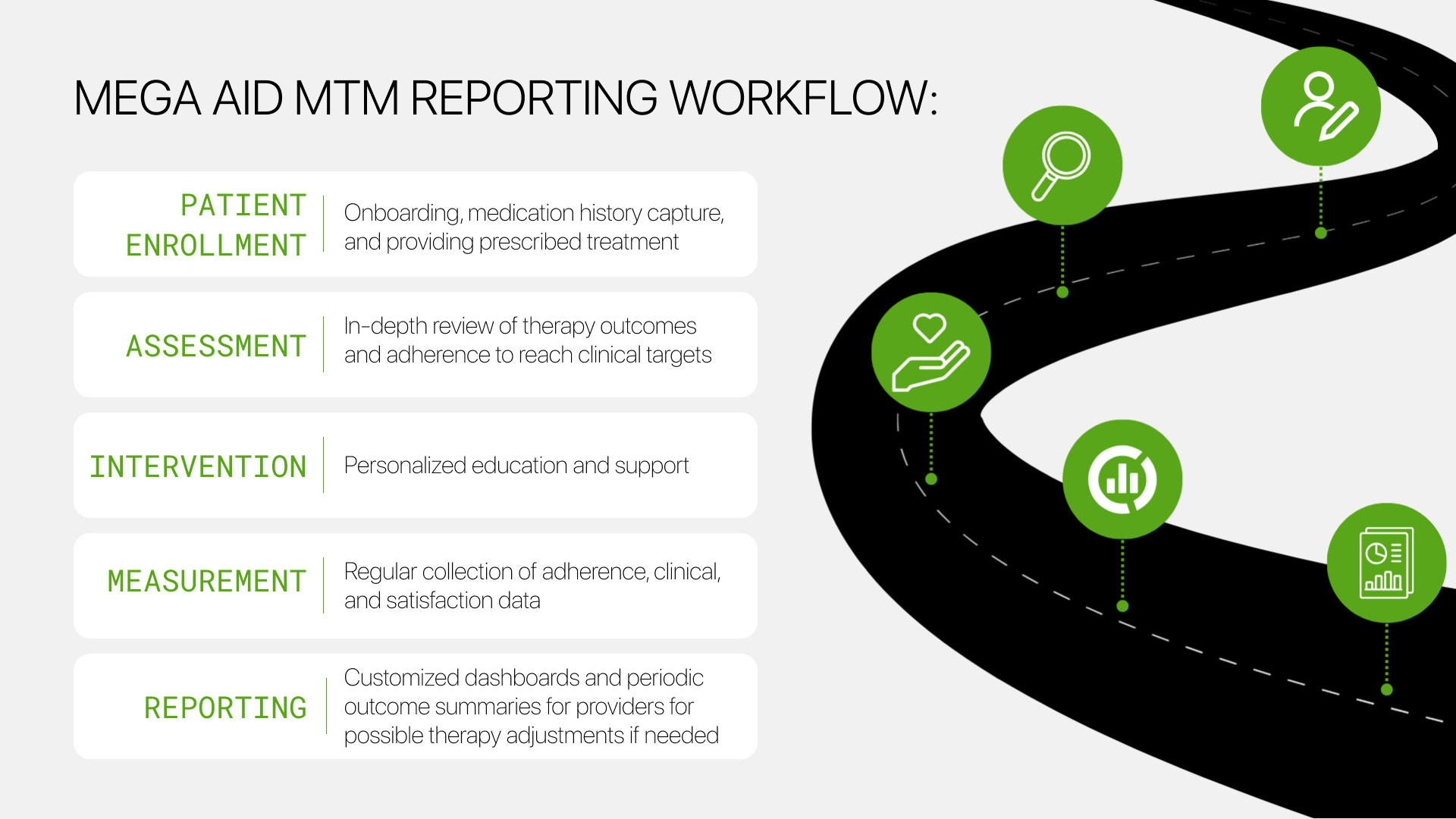
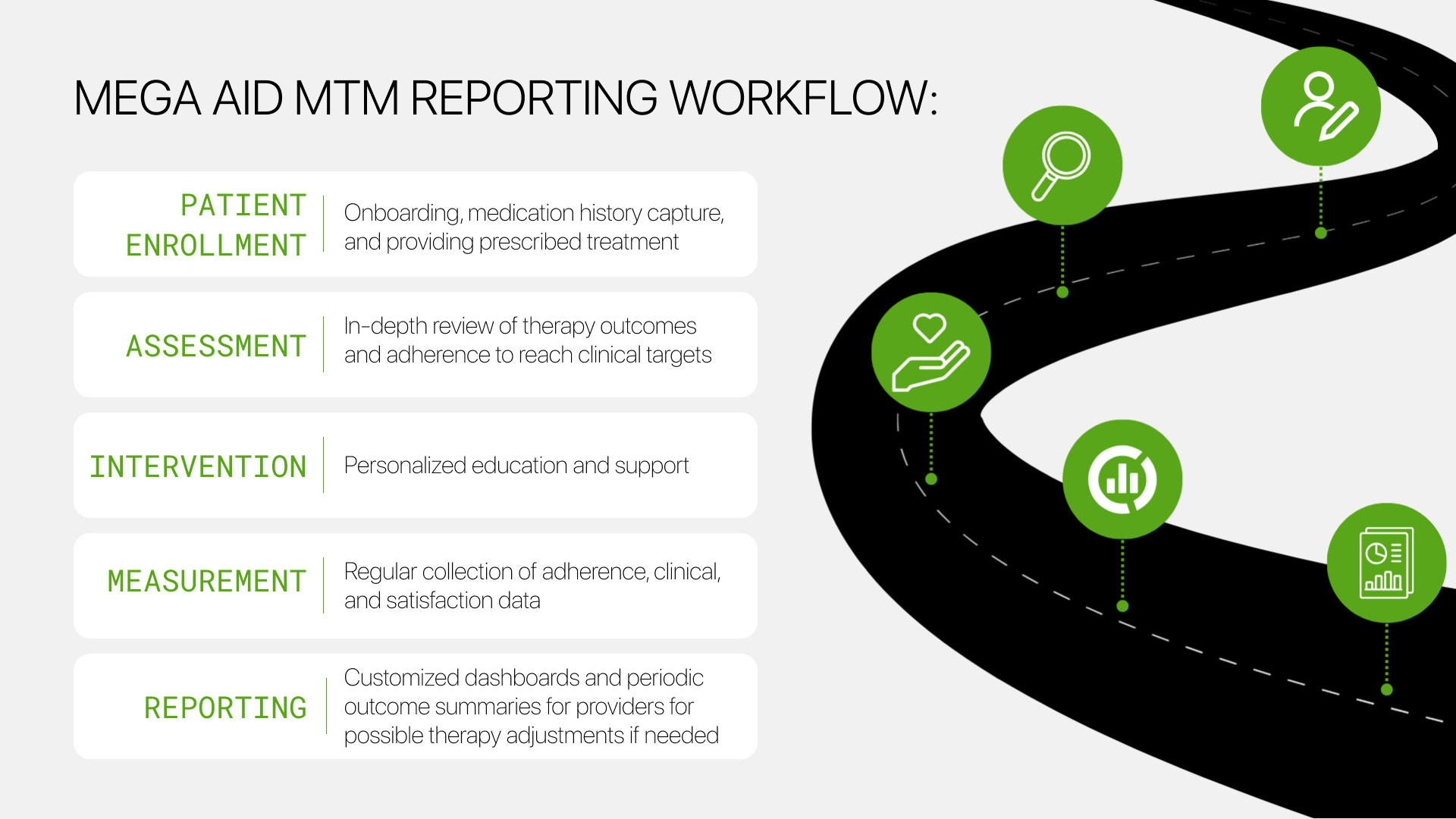
Mega Aid MTM Reporting Workflow
Based on published studies (see references), a combined value-based insurance and MTM program can:
- Increase PDC rates (e.g., from 84.7% to 93.1% in non-adherent patients)
- Significantly reduce gaps in therapy (up to 10.69 fewer days without medication)
- Improve outcomes for specific subgroups (notably female patients)
- Provide cost benchmarks for pharmacy and overall healthcare spend
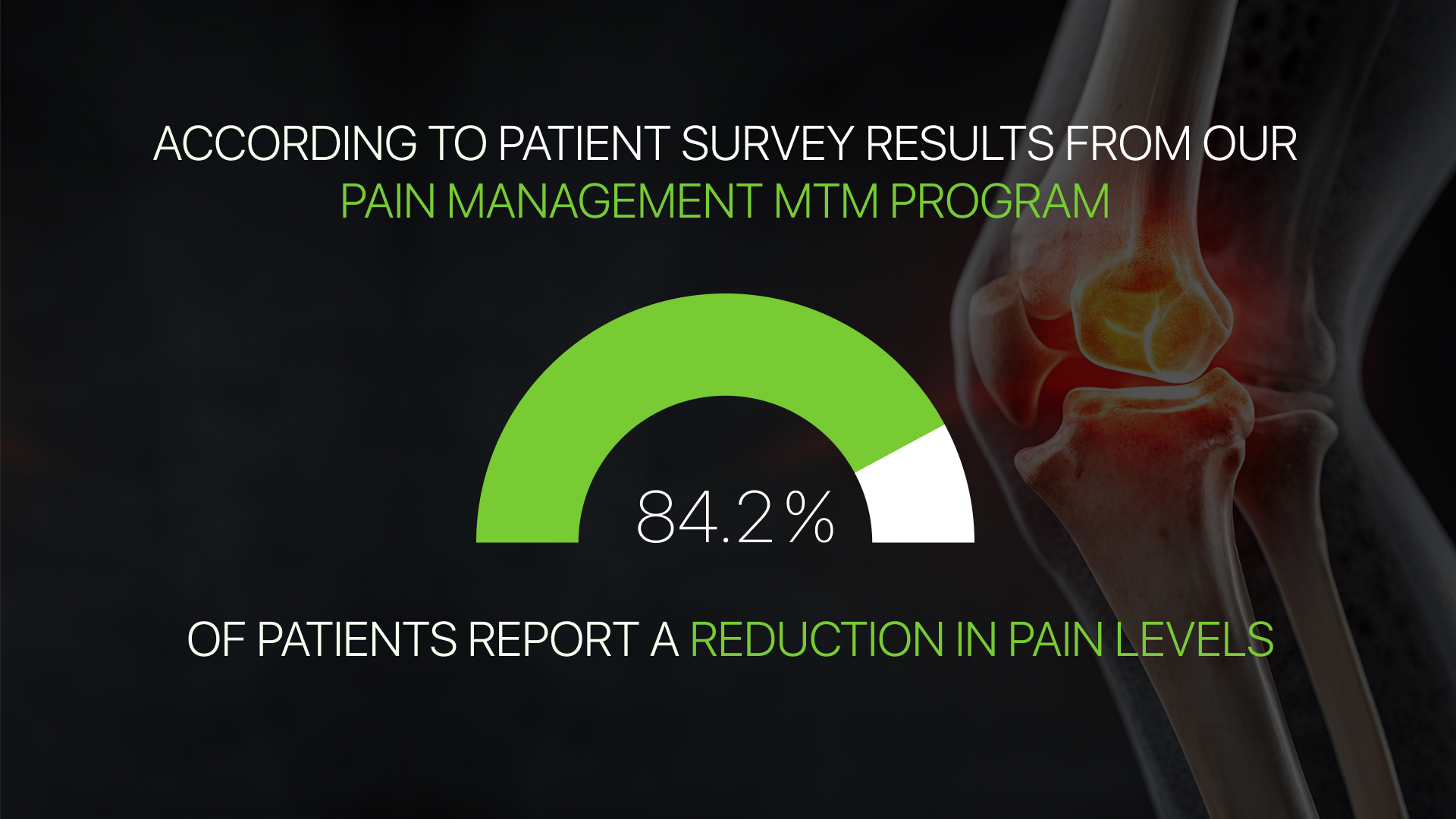
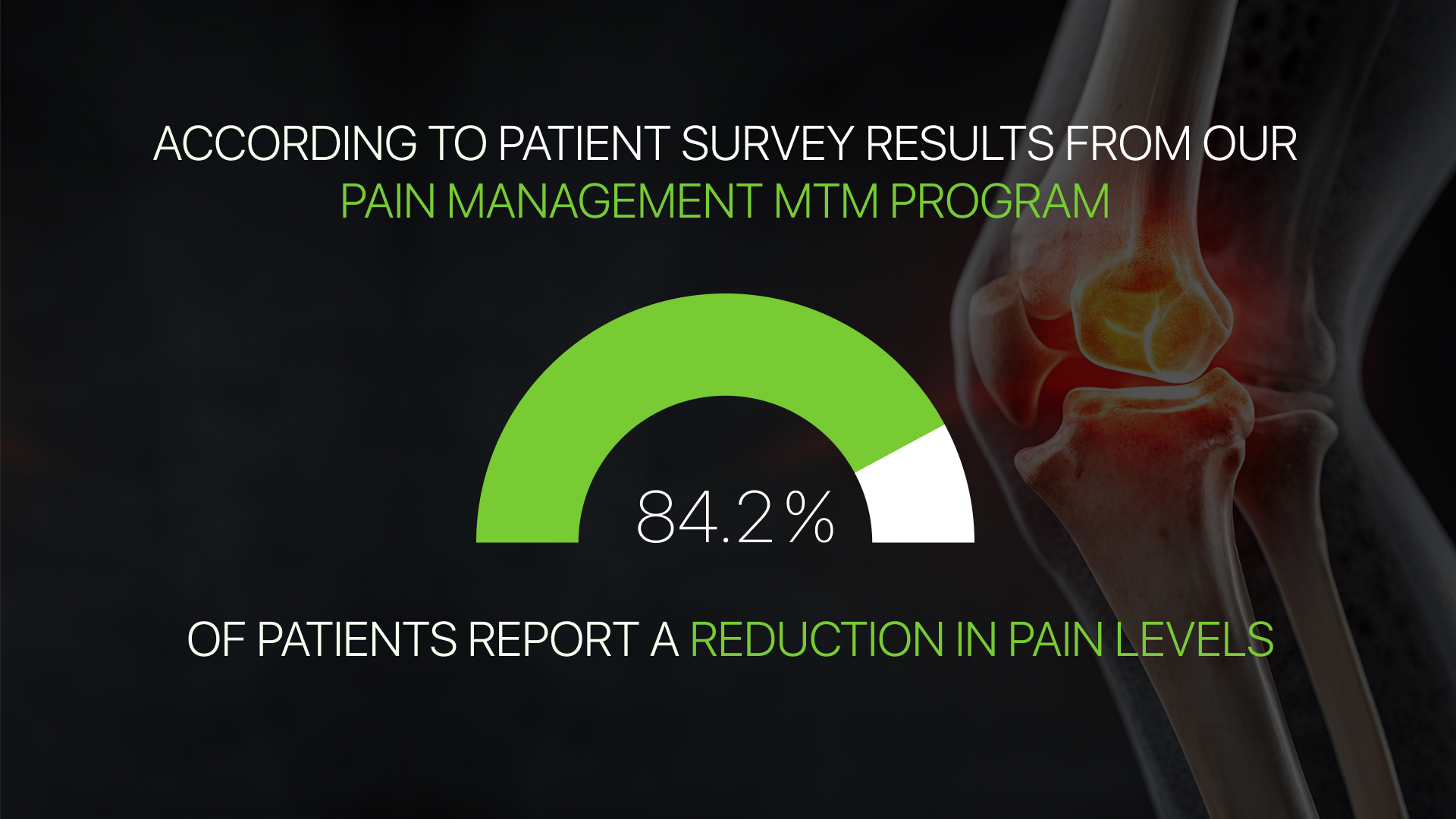
Mega Aid Example:
According to the results of a survey of patients participating in our pain management MTM program, which includes data on pain associated with diabetic neuropathy, arthritis, and inflammatory pain in joints and muscles, 84.2% of patients report a reduction in pain levels.
Example Table: Adherence Metrics Before & After MTM
| Metric | Pre-MTM Intervention | Post-MTM Intervention |
|---|---|---|
| PDC (%) | 84.7 | 93.1 |
| Gaps in Therapy (days) | 15.2 | 4.5 |
Sample Provider Report Sections:
- Patient cohort summary
- Adherence and gap analysis
- Intervention outcomes and follow-up actions
- Recommendations for further care
Frequently Asked Questions
Q: How can Mega Aid’s MTM data be integrated into existing value-based care workflows?
A: Mega Aid structures MTM data so it can align with existing provider, payer, and health system workflows. Reports are designed to support clinical reviews, quality meetings, and value-based performance evaluations by summarizing therapy effectiveness, adherence trends, and intervention outcomes in a format that complements EHR reviews, care coordination discussions, and payer reporting requirements.
Q: Does Mega Aid’s MTM support longitudinal tracking of patient outcomes over time?
A: Yes. Mega Aid’s MTM program emphasizes longitudinal monitoring, allowing providers and care teams to evaluate trends in adherence, symptom improvement, and treatment response over time. This longitudinal view is especially valuable for chronic conditions and value-based programs that reward sustained improvements rather than short-term results.
Q: How does Mega Aid’s MTM reporting support clinical decision-making beyond adherence metrics?
A: In addition to adherence data, Mega Aid’s MTM reporting highlights therapy effectiveness, patient-reported outcomes, tolerance issues, and opportunities for formulation or dosing adjustments. This enables providers to make informed clinical decisions, refine treatment plans, and improve outcomes without relying solely on claims-based or refill-level data.
Q: Is Mega Aid’s MTM reporting suitable for specialty, compounded, or non-standard therapies?
A: Yes. Mega Aid’s MTM program is specifically designed to support compounded and customized therapies that are often excluded from traditional reporting models. By tracking real-world use, patient education effectiveness, and treatment response, Mega Aid provides visibility into therapies that may not be fully captured by standard pharmacy benefit or claims systems.
Q: How does Mega Aid ensure MTM data supports quality, compliance, and audit readiness?
A: Mega Aid operates within PCAB accreditation standards and USP 795/800 compliance, with structured documentation and consistent follow-up processes. MTM interactions, interventions, and outcome tracking are documented to support quality oversight, internal audits, and external reviews tied to value-based or performance-driven care models.
Mega Aid is a PCAB-accredited, USP 795/800 compliant pharmacy specializing in personalized MTM and compounding solutions, serving the greater New York area and New Jersey. Our mission is to optimize outcomes and support value-based healthcare through innovation, collaboration, and robust reporting.

